In a remarkable scientific breakthrough, researchers at Stanford Medicine have successfully recreated a key human sensory pathway in a laboratory dish—an innovation that could reshape how chronic pain is studied and treated.
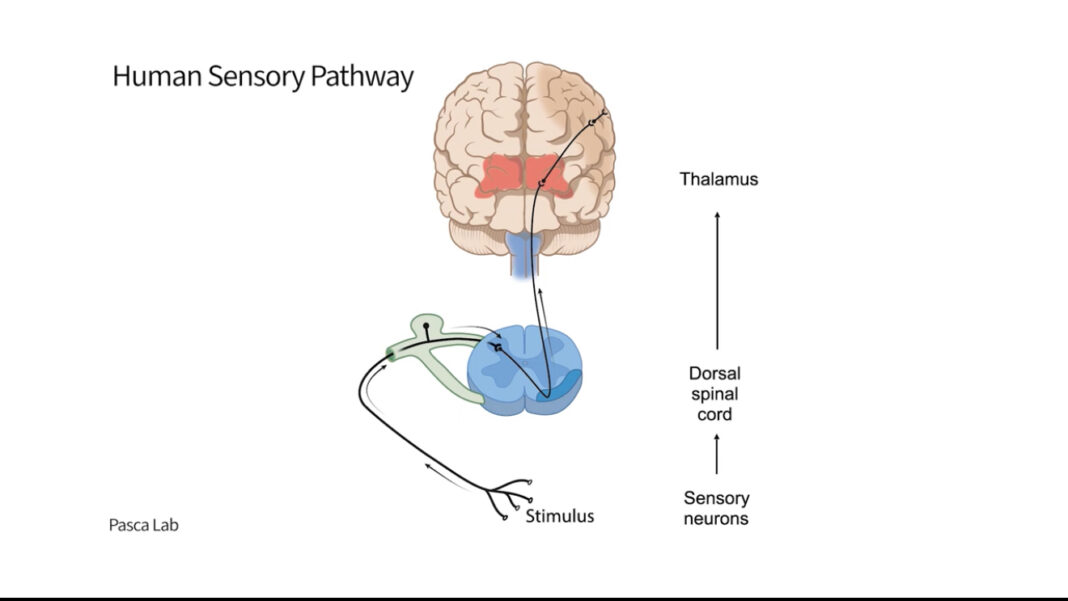
Led by Dr. Sergiu Pasca, a professor of psychiatry and behavioral sciences, the team built a functioning pain circuit using lab-grown “organoids” representing four parts of the human nervous system: the dorsal root ganglion, spinal cord, thalamus, and somatosensory cortex. These were combined into a single unit known as an “assembloid,” which for the first time allowed scientists to observe how pain signals travel from the skin to the brain.
The study, published April 9 in Nature, shows how this model can simulate pain response in real time. When exposed to capsaicin—the active ingredient in chili peppers—the assembloid responded with waves of electrical activity, mimicking how the human body reacts to painful stimuli.
Researchers also explored the genetic basis of pain by modifying the assembloid with a mutation in the Nav1.7 gene, known to influence pain sensitivity. The altered models showed disrupted or heightened activity, offering clues to why some people experience more or less pain than others.
Importantly, the assembloid doesn’t “feel” pain but can transmit signals, making it a powerful, ethical tool for testing new pain treatments without involving live human or animal subjects.
“This model gives us a new, non-invasive way to study pain and develop more targeted therapies,” said Dr. Pasca.
Chronic pain affects over 116 million Americans, and current treatments often fall short. This research offers hope for more effective, personalized solutions in the near future.
Source: Stanford Medicine
A global media for the latest news, entertainment, music fashion, and more.